Stomatitis
This webpage is intended for UK healthcare professionals. If you are not a healthcare professional, please click here.
Introducing the button-free Metoject® PEN
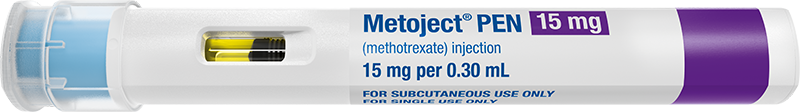
Offering the simplicity of a button-free autoinjector, purpose designed with patient-friendly features
Metoject® PEN For Rheumatology
Metoject PEN® is used to treat active rheumatoid arthritis in adult patients, polyarthritic forms of severe, active juvenile idiopathic arthritis and psoriatic arthritis.1
The National Rheumatoid Arthritis Society (NRAS) describes methotrexate as the ‘gold standard’ disease modifying anti-rheumatic drug (DMARD) for the control of inflammatory arthritis.8
Why use Metoject® PEN to Treat Rheumatoid Arthritis?
Clinical research has shown several benefits of Metoject® PEN and subcutaneous methotrexate administration, including:
 The bioavailability of subcutaneous methotrexate is higher compared to oral methotrexate.1,3
The bioavailability of subcutaneous methotrexate is higher compared to oral methotrexate.1,3In dosages between 7.5mg/m2 and 80mg/m2 body surface area, the bioavailability of subcutaneous methotrexate is nearly 100%, while the mean bioavailability of methotrexate absorbed from the gastrointestinal tract is approx. 70% with considerable inter- and intra-individual deviations.
Subcutaneous administration of methotrexate with Metoject® PEN resulted in a higher relative bioavailability compared to oral administration of methotrexate after single doses of 7.5mg, 15mg, 22.5mg, and 30mg.

Subcutaneous administration is significantly more effective than oral administration.7
A study compared the efficacy of subcutaneous vs. oral methotrexate in patients with active rheumatoid arthritis. At week 24, significantly more patients treated with subcutaneous methotrexate than with oral methotrexate met the American College of Rheumatology criteria (ACR) for 20% improvement (78% versus 70%) and ACR criteria for 70% improvement (41% versus 33%).Patients with a disease duration ≥ 12 months had even higher response rates for the ACR criteria for 20% improvement (89% versus 63%).
The rate of adverse events was similar in all groups.

Patients suffer less frequent and less intense GI discomfort with subcutaneous administration.4
A survey compared the frequency and intensity of nausea and frequency of gastrointestinal discomfort in rheumatoid arthritis patients treated with either oral or subcutaneous methotrexate. The results demonstrated that changing methotrexate dosing from oral to subcutaneous significantly reduced gastrointestinal adverse events.

Methotrexate reduces the risk of cardiovascular diseases.9
In a study of 2044 rheumatoid arthritis patients, methotrexate reduced the risk of composite cardiovascular diseases (CVD) and congestive heart failure, with a trend toward reduced risk of myocardial infarction and stroke.
Methotrexate reduces the risk of cardiovascular diseases in RA patients by 24% and the risk of heart failure by 57%.

Significant improvement in disease activity scores with subcutaneous methotrexate.10
A study demonstrated an early effect of optimal dosing of subcutaneous methotrexate in patients with early rheumatoid arthritis. The research found a significantly larger early improvement in several disease activity scores and higher proportion achieving early Clinical Disease Activity Index (CDAI) and Disease Activity Score (DAS28) remission.
By 6 weeks, 59 % of patients had achieved either DAS28 remission or low disease activity state, with 74 % achieving either state by 12 weeks.
There were no dropouts and few reported headache (3 %), nausea (4 %) and GI symptoms (1 %).
.
Methotrexate for Rheumatoid Arthritis Patient Support Videos
Understanding methotrexate – this video tells you all you need to know about how Methotrexate works, its benefits and possible side-effects.
In this introduction video we are joined by Tracy French, Rheumatology Clinical Nurse Specialist at University Hospitals Bristol. Tracy runs through the ‘ASK’ approach and how to approach your RA journey.
Please visit the National Rheumatoid Arthritis Society’s webpage at nras.org.uk for more rheumatoid arthritis specific information and support
Metoject® PEN Support Materials & Information
Side Effects
Although subcutaneous (vs. oral) methotrexate is more tolerable, very common side effects include1:
Reporting Side Effects
Adverse events should be reported using the forms and information found at yellowcard.mhra.gov.uk
Please also report any adverse events by email to medac drug safety at drugsafety@medac.de
Further Information & Questions
Visit our contact page to submit an enquiryReferences:
- Metoject® Summary of Product Characteristics. [online] Available at: https://www.medicines.org.uk/emc/search?q=metoject#gref/. Last Accessed May 2023
- Müller, R.B. et al. (2015). Effectiveness, tolerability, and safety of subcutaneous methotrexate in early rheumatoid arthritis: A retrospective analysis of real-world data from the St. Gallen cohort. Seminars in Arthritis and Rheumatism, 45(1), pp.28–34.
- Pichlmeier, U., & Heuer, K. U. (2014). Subcutaneous administration of methotrexate with a prefilled autoinjector pen results in a higher relative bioavailability compared with oral administration of methotrexate. Clinical and experimental rheumatology, 32(4), 563–571.
- Kromann, C.B. et al. (2014). Does switching from oral to subcutaneous administration of methotrexate influence on patient reported gastro-intestinal adverse effects? Journal of Dermatological Treatment, 26(2), pp.188–190.
- EU Council Directive 2010/32/EU on the prevention of sharps injuries in the hospital and healthcare sector
- Latex data on file
- Braun, J. et al. (2008). Comparison of the clinical efficacy and safety of subcutaneous versus oral administration of methotrexate in patients with active rheumatoid arthritis: results of a six-month, multicenter, randomized, double-blind, controlled, phase IV trial. Arthritis and rheumatism, 58(1), 73–81.
- Methotrexate and its use in rheumatoid arthritis (RA). [online] Available at: https://nras.org.uk/resource/methotrexate/. Last Accessed May 2023.
- Johnson, T.M. et al. (2021). Investigating changes in disease activity as a mediator of cardiovascular risk reduction with methotrexate use in rheumatoid arthritis. Annals of the Rheumatic Diseases, [online] 80(11), pp.1385–1392.
- O’Connor, A. et al. (2016). The rapid kinetics of optimal treatment with subcutaneous methotrexate in early inflammatory arthritis: an observational study. BMC Musculoskeletal Disorders, 17(1).
- Kanwar, A., Yadav, S. and Dogra, S. (2010). Psoriasis: What is new in nonbiologic systemic therapy in the era of biologics? Indian Journal of Dermatology, Venereology, and Leprology, 76(6), p.622.
- Warren, R.B. et al. (2017). An intensified dosing schedule of subcutaneous methotrexate in patients with moderate to severe plaque-type psoriasis (METOP): a 52 week, multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet, 389(10068), pp.528–537.
- Reich, K. et al. (2020). The value of subcutaneous vs. oral methotrexate: real‐world data from the German psoriasis registry PsoBest. British Journal of Dermatology, 184(4), pp.765–767.
- Generali, E. et al. (2021). Non-adherence and discontinuation rate for oral and parenteral methotrexate: A retrospective-cohort study in 8,952 patients with psoriatic arthritis. Journal of Translational Autoimmunity, 4, p.100113.
